How to Get Tested for Celiac Disease, Accurately
As an Amazon Associate and member of other affiliate programs, I earn from qualifying purchases.
You’re not feeling well. You wonder if your’re a hypochondriac After all you’ve talked to “Dr Google” a hundred times, looking for possibilities and answers. Are you a candidate to be tested for Celiac Disease?
Has a family member been diagnosed, and they’re urging you to get checked out? The idea of having an autoimmune disease is distressing enough. The thought of taking the steps to found out for sure may seem daunting. It’s not a surprise. There are a lot of competing voices out there.
Take a deep breath. I’ll share a bit of my own journey, facts from trustworthy organizations, and try to help you figure out how to best navigate your concerns on being tested for Celiac Disease.
1. Don’t Change Your Diet Before Antibody Testing

I’ve heard so many heart breaking stories of people who’ve stopped eating gluten prior to being tested for Celiac Disease. Maybe they did it on their own because they wanted to feel better. Maybe a doctor told them to stop prior to testing. DON’T DO IT! All of the accurate testing methods we have to date require the consumption of gluten.
Wheat Allergy vs. Celiac Disease. Vs. Gluten Sensitivity
Maybe you’re thinking, “If I feel better eating gluten-free, what’s the difference?” There’s a lot of difference, according to the University of Chicago Celiac Disease Center. There are three medical issues linked to wheat (wheat allergy, Celiac Disease, and Non-Celiac Gluten Sensitivity) that are distinctly different and require different treatments. Celiac Disease has many associated health issues, such as thyroid disease, osteoporosis, and other intestinal issues. It is important to have an accurate diagnosis to make sure you are getting proper follow-up care. Also, the term “gluten allergy” isn’t accurate.
What If It’s Actually Chron’s Disease?
In addition, Crohn’s Disease and Celiac Disease have many overlapping symptoms, and again require different treatments. (I actually know of a young man who was misdiagnosed for years with Celiac Disease when in fact he had Crohn’s. Not fun.) There are over 300 symptoms that are associated with Celiac Disease, which can make it difficult to diagnose. You owe it to yourself to know for certain!
My Doctor is Worthless / Refuses to Test Me
I know that there are plenty of not-so-great doctors out there. I’ve had my fair share. For those living in Michigan, I highly recommend the doctors at Michigan Medicine Celiac Disease Program. The Celiac Disease Foundation also provides a list on their website of doctors, dietitians and other medical professionals that they trust.
2. Ask Your Doctor to Run Some Blood Tests

A. Celiac Disease Antibody Panel
Doctors have tested for Celiac Disease through the years with a variety of blood work tests. As medical science gets better, so do the tests. As of today, the best test is “tTg-IgA”. This is short for Tissue Transglutaminase Antibodies. It is highly accurate and is positive in 98% of those with Celiac Disease. It is also low in what we call “false positives.” This means that it will accurately come back negative in 95% of those who do NOT have Celiac Disease.
What About False Positives and False Negatives?
“There is a risk of a false positive especially for people with associated autoimmune disorders like Type 1 diabetes, chronic liver disease, Hashimoto’s thyroiditis, psoriatic or rheumatoid arthritis and heart failure, who do not have celiac disease.“
Because there is some wiggle room, doctors SHOULD run these additional blood antibody tests-
Endomysial Antibodies (EMA), total serum IgA, and Deamidated Gliadin Protein (DGP)
Also please know, that as great as science is, it is still possible for lab tests to come back with a false negative. If you still feel awful, and especially if you have a family history of Celiac Disease, continue to consult with your doctor. Share this guide from the Celiac Disease Foundation if they seem unsure of what tests to run.
Antibody Testing in the Black Community
Recent research has shown that antibody testing in the Black community is not always accurate. A 2022 study showed that “Eighty percent of Black patients with biopsy-confirmed celiac disease in the registry had TTG test results that were less than the upper limit of normal, compared to about 9 percent of non-Hispanic white patients in the registry.” I urge my Black friends to test for an upper endoscopy, even if antibody testing doesn’t suggest Celiac Disease.
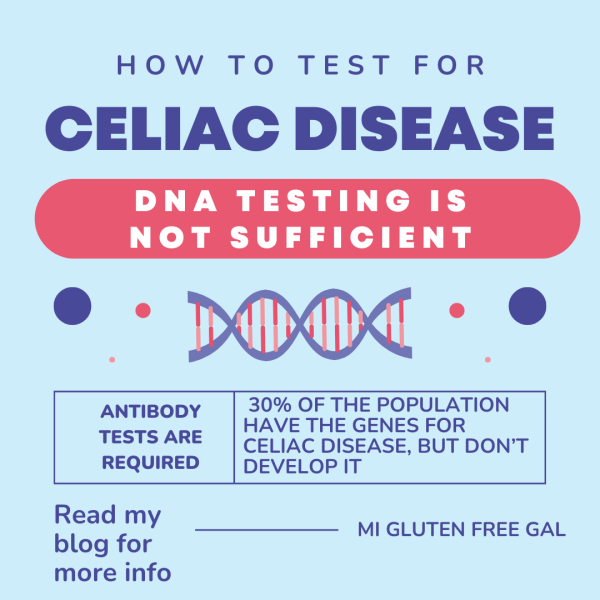
B. Genetic Testing
Scientists have now been able to decipher where the sequences of Celiac Disease reside on our genetic makeup. At this point, genetic testing can only be used to rule out Celiac Disease. Doctors state that if you do not test positive for HLA DQ-2 or HLA DQ-8, you cannot have Celiac Disease.
Unfortunately, simply having those genes don’t mean that you DO have Celiac Disease. A large portion of the population (30%) has those genes, but only 1% of the population develop the disease. Because of this, genetic testing CANNOT be used to diagnose Celiac Disease in those who have already stopped consuming gluten.
3. Meet with a Skilled Gastroenterologist for an Upper Endoscopy

This is me getting ready for a follow-up endoscopy with my new gastroenterologist. A small bowel biopsy, via endoscopy, is the gold standard for being tested for Celiac Disease. I was diagnosed with Celiac Disease in 2001. Fast forward to 2017. My original gastroenterologist followed up only ONCE. He never scheduled follow-up antibody tests to make sure my body was healing. Neither did he check me for osteoporosis, thyroid or other issues. After a move 60 miles away, I decided it was time for a change.
My endoscopy was pretty easy. I didn’t need to drink any junk (that’s for a colonoscopy), and I had to not eat anything for about 10 hours prior to my procedure. Once I was in the procedure room, they were finished in less than 15 minutes. I was under complete anesthesia the whole time. I hear stories by some that weren’t under anesthesia, either because they didn’t want to be or their doctor was foolish.
What Exactly is an Endoscopy?
I’ll explain what an endoscopy is, as that seems it is what makes most people most anxious in being tested for Celiac Disease. During an endoscopy, they stick a small tube with a camera in it to visibly inspect your esophagus, stomach and the duodenum (top part of the intestines.) They also take small bits of tissue, called a biopsy. Tiny, tiny bits of tissue. Small, barely there bits that go under a microscope. These bits are tested and inspected for damaged villi, which are responsible for absorbing our nutrients. This video is great for children who are anxious about underoing an endoscopy.
How Many Samples Should My Doctor Take?
Make sure that your gastroenterologist is taking at least 6 samples from various places in the duodenum. One sample is not enough to make a definitive diagnosis. Celiac Disease can affect one patch of the intestines and not another. More samples are always better. This medical standard in Celiac Disease testing is better explained in the University of Chicago Celiac Disease Center’s explanation of an endoscopsic biopsy.
There may be a day in the future when we will have less invasive ways to diagnose Celiac Disease. But until then, I will personally still advocate for an biopsy via endoscopy. During the biopsy, doctors might notice items of additional concern. For example, my follow-up endoscopy revealed a hiatal hernia.
4. Meet with an Educated Dietitian and Other Resources

So you’ve been poked, prodded, tested and inspected. You’ve been tested for Celiac Disease and the results are positive. Now what on earth do you do? It’s not as simple as “just take gluten out of your diet.” I mean, that’s what we need to do, but it’s a big learning process. What is gluten? Where does it hide? What other nutritional deficiencies should I be concerned about? Can I ever eat pizza again?
Step 1 After Diagnosis – Find a Knowledgeable Dietitian
This is where a good dietitian who is versed in Celiac Disease is a good place to start. I would again use the CDF provider directory to find one a knowledgeable dietitian. Remember, dietitians have to learn A LOT in school, and some may not be well versed in Celiac Disease. I know Gluten Free Watchdog has offered, in the past, to help people find a good dietitian.
Step 2 – Develop a Support System
I always recommend finding a local Celiac Disease support group. You can find some in my list of local and national resources. Many groups have a dietitian who advises their group as well. They are also the people who have been navigating and living with this disease everyday They are the ones who have walked in the shoes that you now find yourself in. They know the emotional side of Celiac Disease.

There are lots of good online resources for those of us who are newly diagnosed. The Gluten Intolerance Group, the Celiac Disease Foundation, and Beyond Celiac are all organizations devoted to helping those with Celiac Disease. They all excel at certain aspects of Celiac Disease management. The University of Chicago Celiac Disease Center is an excellent resource as well. Their “FAQ” section is the biggest searchable question database I’ve ever seen. The offer a free E-book to help you “Jump Start” your gluten-free lifestyle.
Be Careful of Who You Follow Online
There are lots of self proclaimed experts online. Make sure that whomever you are following is providing sound medical advice. While I usually don’t “call out” pages I disagree with, I have reservations about Celiac.com and the Gluten Free Society. The first, as explained by Gluten Dude, has lost its credibilty. The second has always been about making money, and promotes unsound medical advice. Just remember, if someone is spouting something too good to be true, it likely is.
Hopefully I’ve given you some information that’s been helpful in regards to being tested for Celiac Disease. I will state clearly that I’m not a doctor, dietitian, nurse or “certified” medical professional. I am a previous Celiac Disease support group chair and a Celiac Disease advocate. I’m a fellow “gluten free gal,” whose been diagnosed with Celiac Disease for over 20 years.
I’m walking this journey with you, every step of the way.
How were you diagnosed with Celiac Disease? What part was most concerning for you? What insights can you share with those who are about to be tested for Celiac Disease? Please share your thoughts below!
Originally published 2018

Very interesting article. Would value your input, as it seems the medical community has not well defined my condition. As part of my fight against breast cancer, I underwent chemo with seemingly unstoppable diarrhea as a side effect. That cut short my number of treatments from 6 to 4. Months afterwards, I still had diarrhea daily and went to a gastroenterologist. A biopsy taken during a colonoscopy indicated Celiac. Next step, the endoscopy and results were negative for Celiac. I was told to go on a gluten free diet because “it wouldn’t hurt to try.” I felt much better and it has now been 2 years. I still don’t understand this whole thing, because I seem to be able to tolerate white bread (bleached flour) and other times I’ll react violently when I have not eaten gluten. Any idea what might be going on here? Was the chemo a trigger for underlying Celiac or am I not really Celiac at all? (By the way, I also had a colon resection due to diverticulitis) Thanks!
Dear Fellow Margaret,
You have a very interesting situation indeed. It is known in the medical community that “trauma” can trigger the genes that cause Celiac Disease. (Even giving birth, although a positive life experience, is still traumatic to the body.) I would say that it is totally possible that the chemo triggered your Celiac Disease. A few things come into play though in a diagnosis. Theoretically, you should have first been screened for Celiac Disease through a blood antibody test. (Then again, I never was, as I have a family history.) The biopsy needed to have been done on the small bowel, which is normally done through endoscopy. They also needed to have taken 6 samples from different parts of the duodenum. Then those samples needed to have been sent to someone skilled in reading those labs. I know a family whose son is incorrectly diagnosed with Celiac when he actually has Chron’s Disease, which requires a very different direction of treatment.
I would say that if you’re still concerned, and occasionally eating gluten, I would visit a trained physician and have then order a Celiac panel which includes antibody tests for TtG, Iga and the others i outlined above. If the antibody levels come back high, then you can discuss with your doctor on how to proceed from there. The diarrhea could also be from the diverticulitis.
I also need to clearly state that i am not a trained medical professional. I am not a doctor, nurse, dietitian or hold any other medical degree. I hope I was able to give you *some* insight and help. Hope you’re feeling better soon!
Thank you, Margaret! I wish I had had that blood test first, too. It would have simplified things quite a bit. I know Celiac was not even considered when that first colonoscopy was performed, but it seems like that blood test should have been performed before going on a gluten free diet. I understand you aren’t a trained medical professional, but I have found I get much better advice from Celiac and Gluten sensitive folks who live this life.
You’re right this is interesting. I’ve seen Crohn’s disease research that says it can cause small intestine villi flattening. Most people with Crohn’s or suspected Crohn’s can’t tolerate the FODMAPs or other starches in wheat. Also note that wheat is extremely high in glyphosate because they use it as a dessicant before harvesting wheat. Check out the MSDS sheet for glyphosate exposure for misinformation-free data about how that affects people.
If you have a lot of willpower, you can try the SCD diet (Specific Carbohydrate Diet) or GAPS (Gut and Psych Syndrome) Diet, both of which focus on rebuilding the intestinal mucosa.
In cancer they give you a drug for nausea called ondasetron (my mom had breast cancer), it lowers serotonin levels which stops the diarrhea / nausea. However, there is a reboud effect. Serotonin is basically an ‘upper’ so you might also feel muscle stiffness or spasms.
There’s a gut specific drug called dicyclomine that can stop diarrhea and also has a rebound effect. I use it to manage constipation because the rebound effect is perfect for helping me sleep at night without stomach gurgles waking me, and then evacuating in the morning.
Gluten Dude just posted a story from his daughter who conquered vomiting and D with a whole foods diet, you might like it. Doing that is far easier than either SCD or GAPS.
I would add, seek a local support group, but don’t believe all they say. People are individuals and until individualized medicine makes any headway, you’ll have to do a lot of research yourself and decide what to believe. I’ve been to support groups where the leaders were ex-employees of DuPont and swore that glyphosate couldn’t possibly hurt you. Make sure the leaders value your experiences and your instincts. Everyone has an instinct for survival, make sure those supporting you are respecting that.
Be careful of bad advice from Facebook groups. MI Gluten Free Gal’s facebook group is excellent as is my local Raleigh Gluten Free Gang facebook group. Be careful of the national ones. Lots of misinformation, also be careful on reddit. A good test is to see if they like Gluten Free Watchdog’s website, and if they quote registered dieticians a lot.
In countries other than the USA, this process can be tricky. You’ll have to go to a capital city if you’re in a second world country where hospitals are iffy. Ask your local doctor where the experts are in gastroenterology. Every country has some, but you will have to travel. It’s better to travel than get bad advice. Northern Africa has a very high estimated occurrence of Celiac disease, but very few hospitals know how to deal with it, so especially there, find the right person.
Tel Aviv has a Celiac Center and a lot of research comes from Tunisia or Algeria, where people find it nearly impossible to follow the gluten free diet so they are studying what happens to them, and how they manage to live gluten free if they do manage it. Don’t wait to be evaluated and treated, long term exposure to gluten can cause life threatening internal bleeding and organ damage according to reports from N Africa. It’s far from a food preference, it’s survival.
Not all support groups are bad. For example, I lead one. The gastro that previously consulted with our group sent patients to us because the dietitians in the area were so lacking in knowledge.
In 2009 my daughter (4 at the time) was having lots of digestive problems. Her pediatrician and the Peds GI doctor just told us she was constipated and to feed her more fruits veg and whole grains. We are VERY well at that time, so this was all she was eating. I was able to get them to test her for dairy issues, which all came back normal, but when we added dairy back in, she ended up with such a massive runny nose she ended up with a staph infection around her nose from all the blowing. I started researching and I decided to cut gluten and dairy from her diet. I feel like we had her tested, but it was a long time ago. I also cut gluten from my diet so she wasn’t eating the “weird” food alone. We both felt AMAZING after the first few weeks. So we just assumed we had a gluten intolerance.
I’ve recently been looking back through my medical records and I discovered that someone tested and diagnosed me for celiac disease in 2012. Despite the fact I’d been gluten free for 3 years, the test came back positive! However, no one told me about the test or results, so I currently have a referral in to see a gastroenterologist to figure out what the next steps are. So not looking forward to possibly having to do a gluten challenge.